Different migraines require different treatment approaches. Migraine is a debilitating disease that can be further complicated when certain symptoms are present.
In the Migraine in America Symptoms and Treatment (MAST) Study, published in Headache, October 2018, almost 96% (3796/3930) of all respondents had at least one unmet acute migraine need.1 The top 6 unmet needs were rapid onset of attack (65%), disability (56%), sleep-related onset (50%), inadequate 2-hour pain freedom (48%), recurrence within 24 hours (38%), and attack-related nausea.1 As the number of unmet needs increased, so did comorbid conditions and symptom severity.1
The American Headache Society recommends a non-oral triptan formulation for the following patient types:2-4


Migraine-Related Gastroparesis
Gastroparesis, or delayed gastric emptying, as well as nausea and vomiting are frequently part of the migraine symptom profile.5
The autonomic nervous system (ANS) is believed to play a critical role in the connection between migraine and gastrointestinal (GI) dysfunction due to overlapping symptomatology, including nausea, vomiting, dyspepsia, and gastroparesis.6,7 Research suggests that migraine-associated GI symptoms may result from disruptions in the gut-brain axis, involving both central and enteric autonomic pathways.5 These disruptions can lead to altered gastric motility, as seen in delayed gastric emptying during and between migraine attacks.5-7
Delayed gastric emptying can impair medication absorption of drugs with high intestinal permeability, complicating migraine management.5,8
Published papers on the connection between GP and migraine.
A link between gastrointestinal disorders and migraine: Insights into the gut-brain connection.
Aurora SK, Shrewsbury SB, Ray S, Hindiyeh N, Nguyen L. Headache. 2021 Apr;61(4):576-589.
Why triptan treatment can fail: focus on gastrointestinal manifestations of migraine.
Newman LC. Headache. 2013;53 Suppl 1:11-6.
Migraine and gastroparesis from a gastroenterologist’s perspective.
Parkman HP. Headache. 2013;53 (Suppl 1):4-10.
Stratified Care
Treatment guidelines for migraine vary, with step care escalating treatment after failures, and stratified care tailoring initial treatment based on severity.
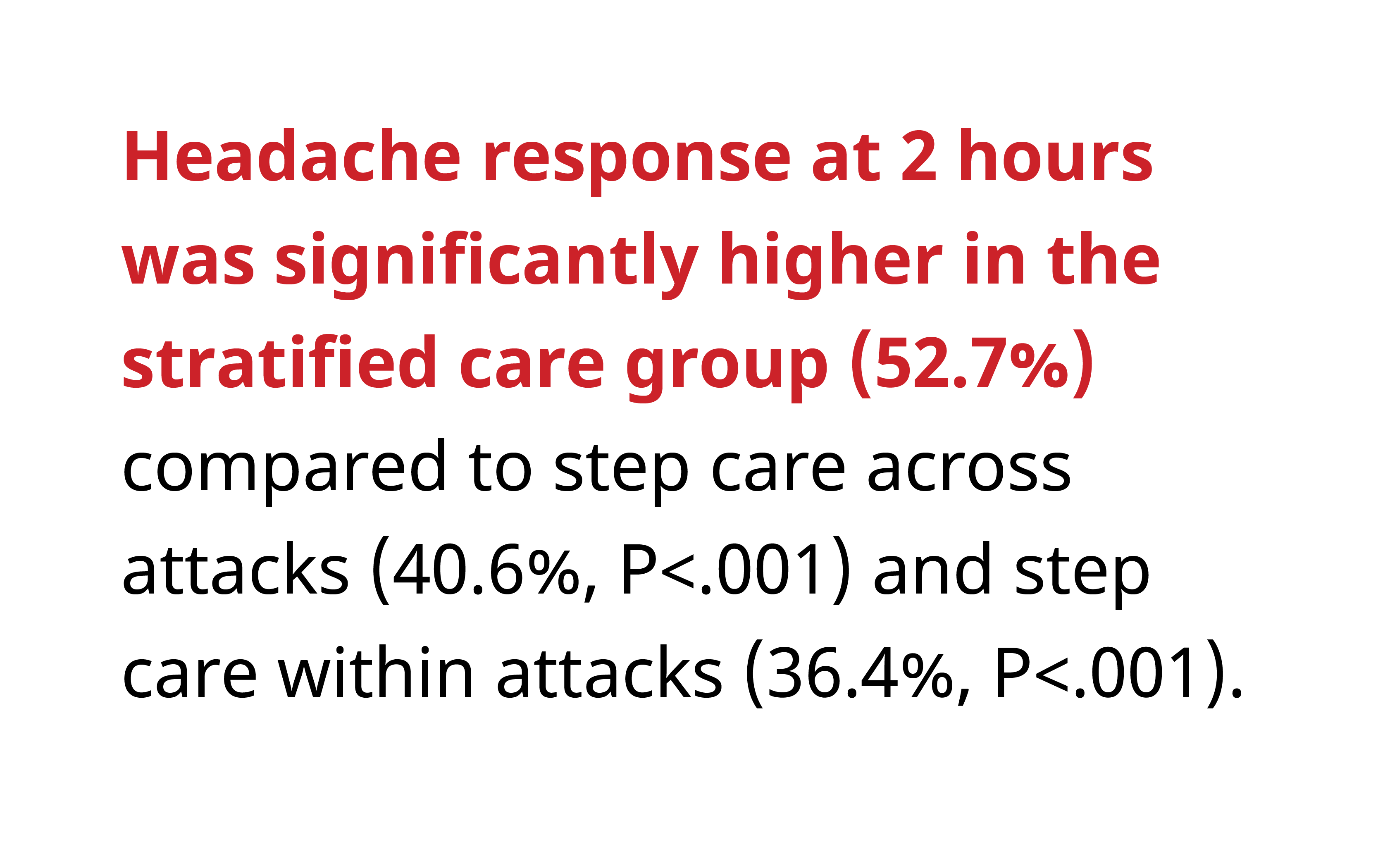
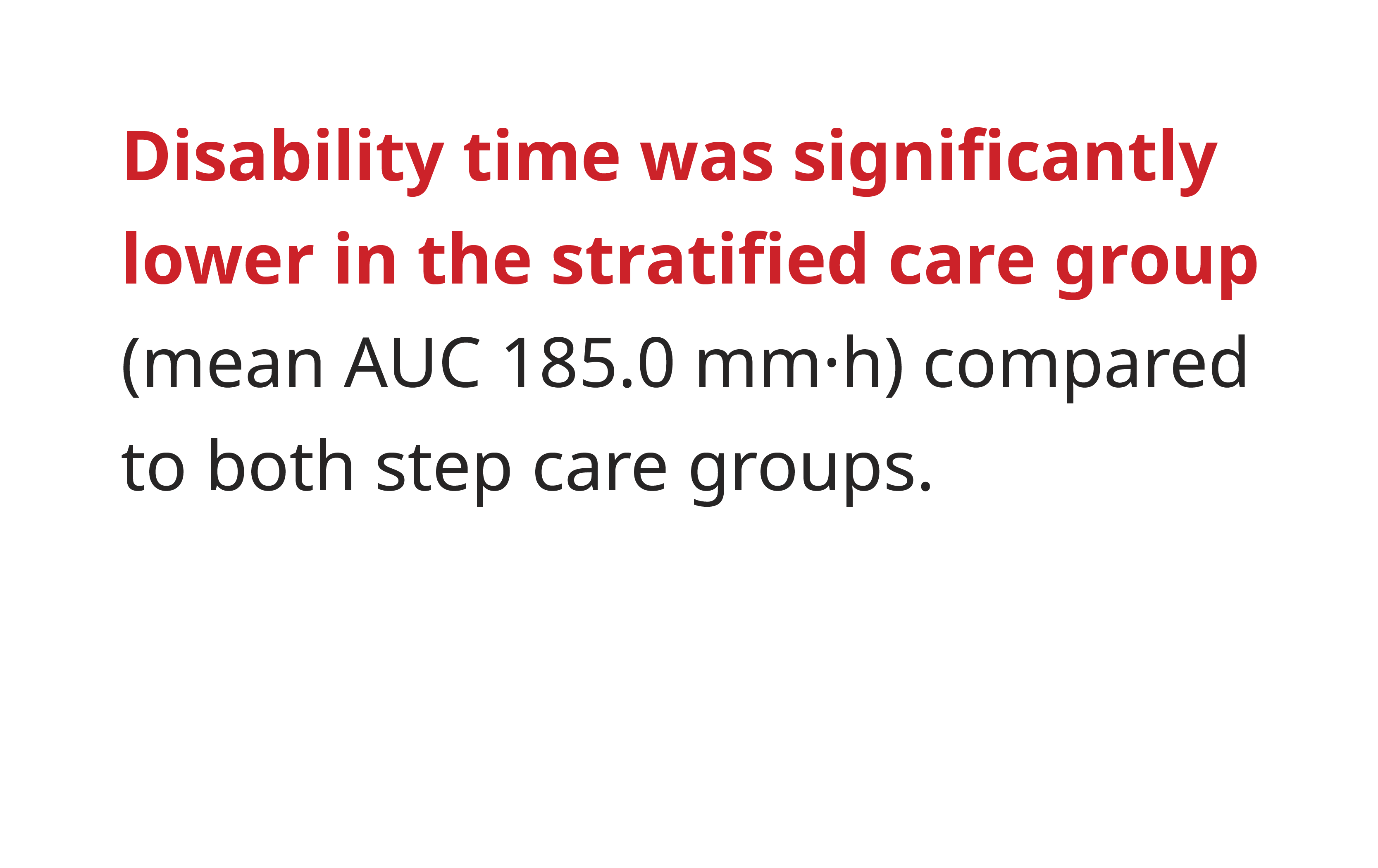
The Disability in Strategies of Care (DISC) study, published in JAMA, 2000, conducted by Lipton et al., compared stratified care, step care across attacks, and step care within attacks for the treatment of migraine.9 This randomized, controlled trial involved 835 adult migraine patients with MIDAS grades II–IV.9 The study concluded that stratified care provides significantly better clinical outcomes than step care strategies, as measured by headache response and disability time.9 Key findings of the study include:9
Optimizing Acute Care
The American Migraine Prevalence and Prevention (AMPP) studies, published in Neurology, 2015, highlight the significant burden of migraine and the need for individualized and optimized acute care strategies. One key takeaway from these studies is that many patients rely on ineffective or delayed treatment, contributing to increased disability and progression to chronic migraine.10-11 Physicians should prioritize early and effective acute treatment, selecting medications based on attack severity, comorbidities, and patient response history.
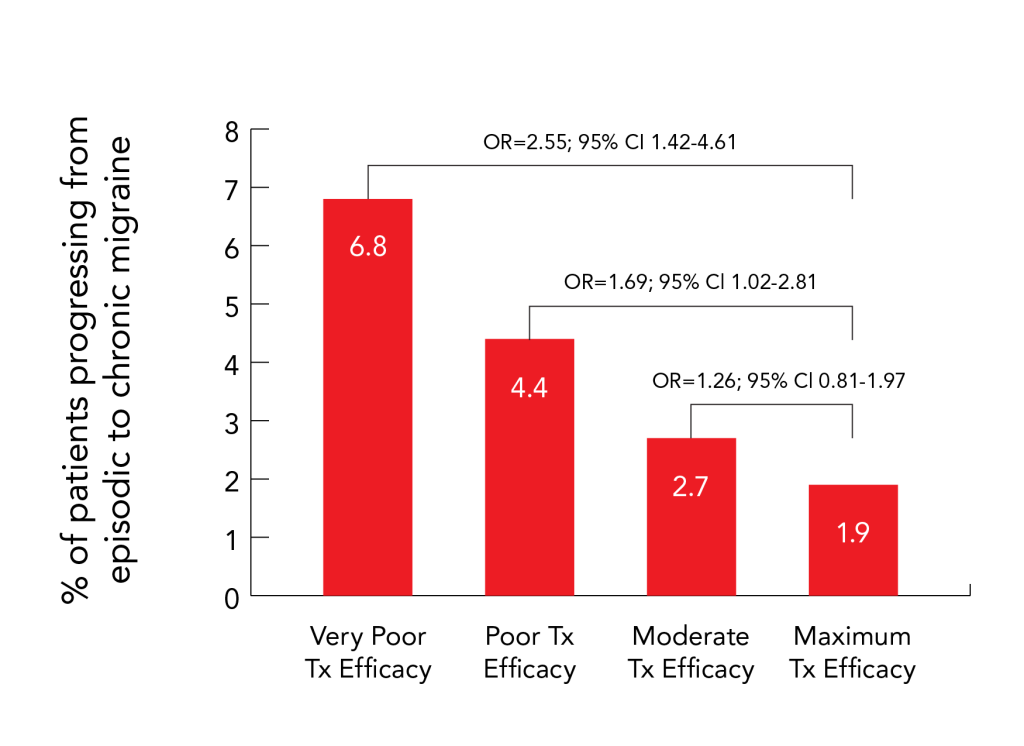
American Migraine Prevalence and Prevention Study12
Suboptimal acute migraine management is linked to a higher risk of progression to chronic migraine within a 12-month period 12
Rates and odds ratios of transition from EM to CM by treatment efficacy category in the fully adjusted model